There is an inimitable story that I recently came across on a medical website. It centres on John, a farmer living in rural Uganda. John is HIV-positive, has no education, and lives with five family members in a mud-walled house that has no electricity. He was diagnosed with HIV in 2005 and started antiretroviral therapy (ART) four months after he developed disseminated herpes zoster (a localised rash) and Kaposi sarcoma (a type of cancer that forms in the skin, lymph nodes, or other organs) with an extremely low and dangerous CD4 count of 151.
What is remarkable about John’s story is that he had close to 100% adherence to his antiretroviral medication (ARVs) despite not owning a watch, an alarm clock, or a basic mobile phone with a built-in alarm clock feature. John was monitored over 89 days and during this period, he took 90% of his prescribed doses of ARVs within ten minutes of 7:20 am and within 17 minutes of 7:20 pm.
So how did John manage to take his medication on time each day? Well, the logical conclusion would be via sunrise and sunset, but John’s solution didn’t rely on a clear sky. Instead, he knew when it was time to take his morning and evening ARVs by listening to a daily radio program that aired at the same time each morning and evening. It is an incredible story and John is proof of how near-perfect adherence can be achieved in resource-limited settings – it just takes a little bit of ingenuity.
HIV Treatment: Times Are Changing
In the early years after the current epidemic was discovered, HIV was something to be greatly feared because back in the late ’80s to early ’90s, contracting the virus was seen as a guaranteed death sentence. To date, HIV and AIDS has killed over 39 million people, but all of this is changing thanks to ground-breaking research, the development of powerful antiretroviral medication, and, of course, technological evolution. HIV has been turned into a manageable chronic illness and HIV-positive persons can live a near-normal lifespan if they take their ART strictly and correctly.
In fact, the current combined effects of ART and technology are working so well that UNAIDS believes that by 2030 AIDS will no longer be a public health threat, meaning that an HIV-free future is becoming an increasing possibility.
Here are five ways innovative technological and medical ingenuity have changed the future of HIV and AIDS forever.
1. m-health – Information at Your Fingertips
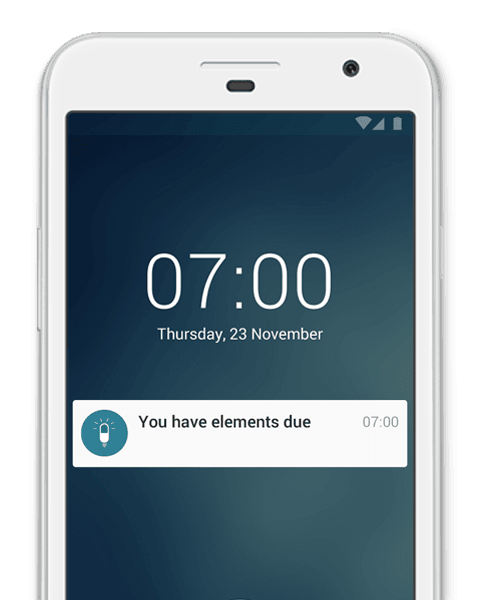
m-health is the use of mobile devices to deliver and improve health services and health-related information. Undoubtedly, the use of mobile phone technology has had one of the greatest impacts on the fight to end HIV and AIDS. Smartphone apps, online messaging services like WhatsApp, and even dating apps all play an important role in providing information and real-time communication with healthcare professionals, encouraging people to get tested and get treatment, and helping people talk about their life with HIV.
An interesting example of this is a community health worker in Malawi, who has made use of SMS services to remind HIV-positive members in her community to attend support groups and HIV health-management classes. In most African countries, broadband services remain unaffordable so access to internet-based communication methods isn’t always a viable option. Therefore, using SMS services is often an effective way of providing services to people in poorer, more rural areas.
2. Telehealth – Remote Access to Healthcare
Telehealth or telemedicine, which is similar to m-health, refers to the use of technology by a healthcare worker to interact and communicate with patients who live far away. The advantage of telehealth, especially for those living in poorer areas, is that it reduces the costs involved in accessing adequate healthcare. For many impoverished people, traveling to clinics is often an expensive or impossible option, so telehealth services make it possible for people to access information and advice.
Priscilla Chomba-Kinywa developed a project in Zambia called U-Report, which uses SMS services to promote sex education to young people. The project includes round-the-clock trained counsellors who are on hand to answer questions on HIV, sexually transmitted infections, and other reproductive health issues.
Other posts you may be interested in on the MyTherapy blog:
- My Husband Is Living with HIV: Poppy’s Love Story
- The Very Best Apps for Seniors - From Accessibility to Entertainment
3. Innovative Smartphone Apps Helping Tackle HIV
There is a myriad of smartphone apps that provide all sorts of services, information, and practical tools for people infected and affected by HIV. Statistics from 2016 indicate that approximately 95% of the world’s population live in an area covered by a mobile cellular network and that there are more than seven billion mobile phone subscriptions worldwide.
With such overwhelming statistics, it comes as no surprise that app developers have taken maximum advantage of this trend. Apps, targeted at HIV-positives persons or those taking pre- or post-exposure prophylaxis, can help people better manage their treatment plans, connect them to healthcare workers and HIV-positive communities, and provide important information on developments and research. Some interesting apps include:
- The Liverpool HIV iChart app provides up-to-date information on possible drug interactions between ARVs and other prescription drugs.
- The Aviro HIV/AIDS Clinical Mentor mobile app, available in South Africa, acts as a real-time mentor for healthcare professionals administering ARV treatment to the patient during the appointment. The app provides immediate feedback and guidance to the healthcare professional, ensuring that the patient receives reliable, effective care.
- The HIV RISK Calculator is an educational app that tells you how risky your sexual activities are and gives you advice on how to perform sexual activities safely. It also tells you where and how to get tested.
- If you’re looking for HIV- and AIDS-related services near any location of your choice, then the HIV Testing Sites and Care Services Locator will do the job. The app is a location-based search tool that allows you to find testing services, health centres, and other service providers based on your current location or any location you choose.
- Medication can be pricey, so the GoodRx (currently available in the USA) app wants to help you save time and money by helping you find the most cost-effective option for any prescription you need to fill.
4. Inventive Ways of Testing For HIV
In order to create an HIV-free future, it is crucial that people get tested and know their status. The UNAIDS has come up with the so-called 90-90-90 target, where 90% of all HIV-positive persons know their status, 90% of these HIV-positive persons are on ART, and 90% of these people on ART achieve viral suppression (the point where the virus becomes undetectable and cannot be transmitted).
It is becoming easier and easier to test for HIV (especially with the rapid test) and many countries offer free testing and counselling services. Researchers at the Colombia University have developed a dongle that can collect a drop of blood and analyse it for the antibodies that fight HIV. The dongle is connected to either a smartphone or tablet via the audio jack and the specific app will analyse the result and give a diagnosis within 15 minutes.
Home test kits have also become a possibility in recent years and many people turn to this kind of testing for more privacy. There are two types of tests you can do at home, the HIV postal test and the HIV self-test. With the postal test, you simply need to take a sample of your blood or saliva and send it to a laboratory. You will then receive your result via a phone call.
With the self-test kit, you take your own blood sample (via a small prick) and the testing kit will give you your status almost immediately. For the most part, HIV home-test kits are extremely reliable, but if you do receive a positive result from the kit, it is important you see a healthcare professional for a confirmation test. While these types of tests can be useful and private, it is imperative, though, that you have someone with you for emotional support. That is why tests done at clinics are preferred because a healthcare professional will be on hand for counselling and treatment initiation if the result is positive.
5. Modern Drugs Preventing HIV
There are several ways in which ARVs can be used to prevent the transmission of HIV. Two of these ways are: pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP).
PrEP refers the use of an antiretroviral drug called Truvada to protect an HIV-negative person from HIV infection. This drug is particularly helpful to persons who are at high-risk for HIV infection (sex workers, for example). Truvada is taken daily (in single-pill, oral form) and research indicates that this pill is between 90% to 99% effective at preventing transmission via sexual activity (if it is taken regularly as prescribed). Post-exposure prophylaxis (PEP) is when ARVS are given to an HIV-negative person after he/she has possibly been exposed to the virus (via a needle-stick injury or unprotected sex, for example).
An interesting app:
The PrEP Locator app was developed to help people in the USA search for PrEP providers according to their zip code, state, or address. The app then also filters out services that do not offer PrEP to those who have no medical insurance.
HIV: What the Future Holds
The average lifespan of someone who acquired HIV around two decades ago was 12 years. Today, those who are HIV-positive are expected to have a near-normal lifespan and a productive, healthy life so long as they continue to take their antiretroviral treatment as prescribed. It goes without saying that modern antiretroviral treatment is nothing short of a miracle.
Years ago, no one would have thought it was possible to have medication that could help HIV-positive persons live normal, healthy lives. In fact, three years ago, no one really thought it was possible to reach the UNAIDS’ 90-90-90 targets. Yet here we are, just a few years later, with incredible statistics: a record 19.5 million people are accessing ART and for the first time, more than half of all people living with HIV are on treatment. In Africa, Botswana is incredibly close to reaching the 90-90-90 target for testing, treatment, and viral suppression and is a leading example of what can happen, even in poorer or undeveloped countries, when free ART is given to people.
The 90-90-90 targets are, of course, ambitious and they require immense global solidarity, continued technological and medical innovation, and shared responsibility on all levels to achieve these targets and work towards an HIV-free future. The very first step to this future is to get tested. There is no need to fear a positive diagnosis anymore: HIV is now a chronic condition, not a death sentence, and can be managed well with adherence to antiretroviral treatment. However, if we do really want to see a future free of HIV and AIDS, then it is important that we remain educated, understand how the virus works and is transmitted, and practice safe sex and hygiene.
UNAIDS wants to see an HIV-free by 2030. Are you in?
Take a look at some of the other posts on the MyTherapy blog: